Sometimes proponents of
pseudoscience embrace nonsense, but other times they propose plausible-sounding ideas that are wrong because the numbers don’t add up. For example, suppose you are discussing with your friend about the biological effects of power-line magnetic fields. Your friend might say something like this:
“You keep claiming that magnetic fields don’t have any biological effects. But suppose it’s not the magnetic field itself, but the electric field induced by the changing magnetic field that causes the effect. We know an electric field can stimulate nerves. Perhaps power-line effects operate like transcranial magnetic stimulation, by inducing electric fields.”
Well, there’s nothing absurd about this hypothesis. Transcranial magnetic stimulation does work by creating electric fields in the body via electromagnetic induction, and these electric fields can stimulate nerves. The qualitative idea is reasonable. But does it work quantitatively? If you do the calculation, the answer is no. The electric field induced by a power line is less than the endogenous electric field associated with the
electrocardiogram. You don’t have to perform a difficult, detailed calculation to show this. A
back-of-the-envelope estimation suffices. Below is a new homework problem showing you how to make such an estimate.
Section 9.10
Problem 36 ½. Estimate the electric field induced in the body by a power-line magnetic field, and compare it to the endogenous electric field in the body associated with the electrocardiogram.
(a) Use Eq. 8.25 to estimate the induced electric field, E. The magnetic field in the vicinity of a power line can be as strong as 5 μT (Possible Health Effects of Exposure to Residential Electric and Magnetic Fields, 1997, Page 32), and it oscillates at 60 Hz. The radius, a, of the current loop in our body is difficult to estimate, but take it as fairly large (say, half a meter) to ensure you do not underestimate the induced electric field.
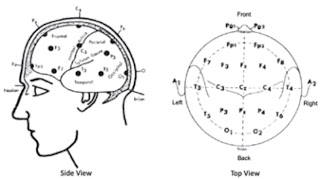
(b) Estimate the endogenous electric field in the torso from the electrocardiogram, using Figures 7.19 and 7.23.
(c) Compare the electric fields found in parts (a) and (b). Which is larger? Explain how an induced electric field could have an effect if it is smaller than the electric fields already existing in the body.
Let’s go through the solution to this new problem. First, part (a). The amplitude of the magnetic field is 0.000005 T. The field oscillates with a period of 1/60 Hz, or about 0.017 s. The peak rate of change will occur during only a fraction of this period, and a reasonable approximation is to divide the period by 2π, so the time over which the magnetic field changes is 0.0027 s. Thus, the rate of change
dB/dt is 0.000005 T/0.0027 s, or about 0.002 T/s. Now use Eq. 8.25,
E =
a/2
dB/dt (ignore the minus sign in the equation, which merely indicates the
phase), with
a = 0.5 m, to get
E = 0.0005 V/m.
Now part (b). Figure 7.23 indicates that the
QRS complex in the electrocardiogram has a magnitude of about
ΔV = 0.001 V (one millivolt). Figure 7.19 shows that the distance between leads is on the order of
Δr = 0.5 m. The magnitude of the electric field is approximately
ΔV/
Δr = 0.002 V/m.
In part (c) you compare the electric field induced by a power line, 0.0005 V/m, to the electric field in the body caused by the electrocardiogram, 0.002 V/m. The field produced by the ECG is four times larger. So, how can the induced electric field have a biological effect if we are constantly exposed to larger electric fields produced by our own body? I don’t know. It seems to me that would be difficult.
 |
Hart and Gandhi (1998)
Phys. Med. Biol.,
43:3083–3099.
|
But wait! Our calculation in part (b) is really rough. Perhaps we should do a more detailed calculation. Rodney Hart and
Om Gandhi did just that (
“Comparison of cardiac-induced endogenous fields
and power frequency induced exogenous fields in
an anatomical model of the human body,” Physics in Medicine & Biology, Volume 43, Pages 3083–3099, 1998). They found that during the QRS complex the endogenous electric field varied throughout the body, but it is usually larger than what we estimated. It’s giant in the heart itself, about 3 V/m. All through the torso it’s more than ten times what we found; for instance, in the intestines it’s 0.04 V/m. Even in the brain the field strength (0.014 V/m) is seven times larger than our estimate (0.002 V/m).
Moreover, the heart isn’t the only source of endogenous fields (although it’s the strongest). The brain, peripheral nerves, skeletal muscle, and the gut all produce electric fields.
In addition, our calculation of the induced electric field is evaluated at the edge of the body, where the current loop is largest. Deeper within the torso, the field will be less. Finally, our value of 5 μT is extreme. Magnetic fields associated with power lines are usually about one tenth of this. In other words, in all our estimates we took values that favor the induced electric field over the endogenous electric field, and the endogenous electric field is still four times larger.
What do we conclude? The qualitative mechanism proposed by your friend is not ridiculous, but it doesn’t work when you do the calculation. The induced electric field would be swamped by the endogenous electric field.
The moral of the story is that proposed mechanisms must work both qualitatively and quantitatively. Doing the math is not an optional step to refine your hypothesis and make it more precise. You have to do at least an approximate calculation to decide if your idea is reasonable. That’s why
Russ Hobbie and I emphasize solving toy problems and estimation in
Intermediate Physics for Medicine and Biology. Without estimating how big effects are, you may go around saying things that sound reasonable but just aren’t true.