|
| Selig Hecht, History of the Marine Biological Laboratory, http://hpsrepository.asu.edu/handle/10776/3269. |
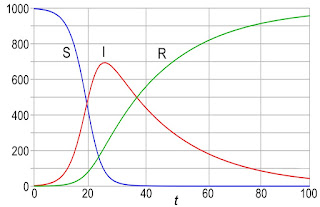
Intensely interested in the relation of light quanta (photons) to vision. Reexamining earlier measurements of the minimum threshold for human rod vision, he and his colleagues confirmed that vision requires only fifty to 150 photons. When all allowances had been made for surface reflections, the absorption of light by ocular tissues, and the absorption by rhodopsin (which alone is an effective stimulant), it emerged that the minimum visual sensation corresponds to the absorption in the rods of, at most, five to fourteen photons. An entirely independent statistical analysis suggested that an absolute threshold involves about five to seven photons. Both procedures, then, confirmed the estimation of the minimum visual stimulus at five to fourteen photons. Since the test field in which these measurements were performed contained about 500 rods, it was difficult to escape the conclusion that one rod is stimulated by a single photon.Wald also describes the coauthor on the study, Shlaer.
Among Hecht’s first students was Simon Shlaer, who became Hecht’s assistant in his first year at Columbia and continued as his associate for twenty years thereafter. A man infinitely patient with things and impatient with people, Shlaer gave Hecht his entire devotion. He was a master of instrumentation, and though he also had a keen grasp of theory, he devoted himself by choice to the development of new technical devices. Hecht and Shlaer built a succession of precise instruments for visual measurement, among them an adaptometer and an anomaloscope that have since gone into general use. The entire laboratory came to rely on Shlaer’s ingenuity and skill. “I am like a man who has lost his right arm,” remarked Hecht on leaving Columbia—and Shlaer—in 1947, “and his right leg.”Hecht and Shlaer both contributed to the war effort during the Second World War.
In his Columbia laboratory, Hecht instituted investigations of human dark adaptation, brightness discrimination, visual acuity, the visual response to flickered light, the mechanism of the visual threshold, and normal and anomalous color vision. His lab also made important contributions regarding the biochemistry of visual pigments, the relation of night blindness to vitamin A deficiency in humans, the spectral sensitivities of man and other animals, and the light reactions of plants—phototropism, photosynthesis, and chlorophyll formation.
Throughout the late years of World War II, Hecht devoted his energies and the resources of his laboratory to military problems. He and Shlaer developed a special adaptometer for night-vision testing that was adopted as standard equipment by several Allied military services. Hecht also directed a number of visual projects for the Army and Navy and was consultant and advisor on many others. He was a member of the National Research Council Committee on Visual Problems and of the executive board of the Army-Navy Office of Scientific Research and Development Vision Committee.
 |
| Explaining the Atom, by Selig Hecht. |
An obituary in Nature by Maurice Henri Pirenne
concludes
The death of Prof. Selig Hecht in New York on September 18, 1947, at the age of fifty-five, deprives the physiology of vision of one of its most outstanding workers. Hecht was born in Austria and was brought to the United States as a child. He studied and worked in the United States, in England, Germany and Italy. After a broad biological training, he devoted his life to the study of the mechanisms of vision, considered as a branch of general physiology. He became professor of biophysics at Columbia University and made his laboratory an international centre of visual research.