|
Ungar et al. (1986) Ann.
Biomed. Engin., 14:437–450. |
In Chapter 7 of
Intermediate Physics for Medicine and Biology,
Russ Hobbie and I discuss
electrical stimulation of nerves. One of the end-of-the-chapter homework problems asks the students to
Design a stimulator that will result in one-way propagation… For an application of such [a device] during functional electrical stimulation, see Ungar et al. (1986).
The reference is
Ungar IJ, Mortimer JT, Sweeney JD (1986) “Generation of Unidirectionally Propagating Action Potentials Using a Monopolar Electrode Cuff,” Annals of Biomedical Engineering, Volume 14, Pages 437–450.
The abstract to their article states
Unidirectionally propagating action potentials, which can be used to implement transmission failure on peripheral nerve through “collision block,” have been generated electrically on cat myelinated peripheral nerve using a monopolar electrode cuff with the conductor positioned closest to the “arrest” end of the cuff. A single cathode located at least 5 mm from the arrest end resulted in unidirectional propagation with minimal current and charge injection. The range of stimulus current values that produced unidirectional propagation increased with increases in longitudinal asymmetry of cathode placement over the range of asymmetries tested (1.7:1 to 7:1). The stimulus current pulse that minimized charge injection was quasitrapezoidal in shape with a plateau pulse width of approximately 350 μsec and an exponential trailing phase having a fall time (90%–10%) of approximately 600 μsec. These parameters were found to be independent of cuff geometry. Arrest efficiency was not degraded using a cuff of sufficient internal diameter to prevent nerve compression in chronic implantation. The critical current density within the extracellular space of the electrode cuff required to produce conduction failure at the arrest end was estimated to be 0.47 ± 0.08 mA/mm2.
I’ll explain how to make a one-way stimulator using the illustration below, adapted from Ungar et al.’s Figure 1.
 |
The design of a one-way neural stimulator.
Adapted from Fig. 1 of Ungar et al. (1986).
|
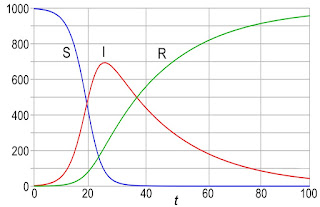
The nerve (blue) is threaded through a cylindrical insulating cuff (red), which resembles a short segment of a plastic drinking straw. The cathode (green) is inside the cuff; it stimulates the action potential. The anode (not shown) is far away. Current (purple curves) comes out of the cathode and enters the nerve axons, depolarizing them. Once it reaches the end of the cuff the current spreads out as it returns to the distance anode. Current there leaves the axons, hyperpolarizing them, and lowering their transmembrane potential. The locations where the axons are hyperpolarized are labeled the virtual anodes.
The key to making a one-way stimulator is to place the cathode off-center in the cuff. Most of the current leaves the cuff through the end nearest the cathode (right end), so the current density is stronger there (the purple current lines are crowded together). Only a small fraction of the current leaves the cuff through the end farther from the cathode (left end), so the virtual anode is weaker there.
Depolarization under a cathode excites an action potential, which then propagates outward in both directions (left and right). If, however, the stimulus strength is strong enough, the hyperpolarization at a virtual anode can block propagation. If the current has the correct strength, the stronger virtual anode on the right will block propagation, while the weaker virtual anode on the left won’t. In that case, an action potential will propagate to the left (the escape end of the stimulator) but will not propagate to the right (the arrest end).
Ira Ungar and his collaborators were able to test their stimulator for different cathodal current strengths. For a very weak stimulus, the cathode is below threshold and no action potential is excited. For a moderately weak stimulus, the cathode excites an action potential that then propagates to both the left and the right; both virtual anodes are too weak to block propagation. For a moderately strong stimulus, the right virtual anode is strong enough to block the action potential and you have one-way propagation. For a very strong stimulus, both ends block propagation, and no action potential leaves the stimulator.
Why construct a one-way stimulator? Suppose you have a nerve that’s constantly firing action potentials, causing unwanted muscle contraction (
spasticity). You could stop the downstream propagation of those action potentials by electrically stimulating action potentials further downstream. The stimulated action potentials propagating upstream will collide with the original action potentials propagating downstream, annihilating them (colliding action potentials can’t pass through each other because they’re each followed by a region of refracotoriness). This works great unless your stimulator sends its own volley of action potentials propagating downstream to excite the muscle. To avoid this problem, you need a one-way stimulator, so you only excite action potentials propagating upstream to block those causing the trouble, but none propagating downstream.
The senior author on this article was
J. Thomas Mortimer, now emeritus professor in the
Neural Engineering Center at
Case Western Reserve University. He earned his PhD from Case and then spent his entire career there. He has developed an online
Applied Neural Control Toolkit to teach how nerves work. I heard Mortimer speak during one of the
Neural Prosthesis Workshops at the
National Institutes of Health; he was inspirational.
Mortimer and his team’s development of a one-way stimulator is a classic example of how physics and engineering can contribute to medicine and biology.