|
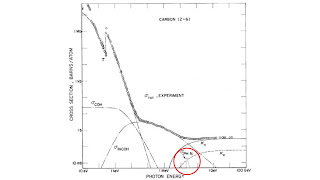
| The Meaning of Everything, by Simon Winchester. |
Rather than describe a typical OED entry, I’ll show ten examples using words drawn from Intermediate Physics for Medicine and Biology.
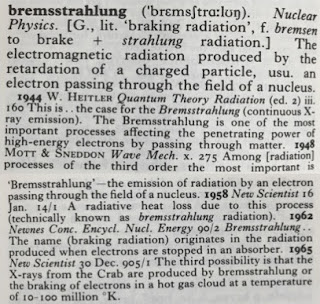
bremsstrahlung
candela
The origin of candela is from Latin (L.). IPMB and Wikipedia define the candela as lumen per steradian. I don’t see the solid angle connection listed in the OED.
chronaxie
Russ Hobbie and I spell chronaxie ending in -ie, which is the most common spelling, although some end it in -y. Chronaxie is from a French (F.) term that appeared in an 1909 article by Louis Lapicque, cited in IPMB.
cyclotron
My favorite part of an OED entry are the quotations illustrating usage. Several quotes are provided for cyclotron. The first is from a 1935 Physical Review article by Ernest Lawrence, the cyclotron’s inventor. XLVIII is the volume number in Roman numerals, and 495/2 means the quote can be found on page 495, column 2.
defibrillation
Two definitions of defibrillation exist. IPMB uses the word in the second sense: the stopping of fibrillation of the heart. Other forms of this medical (Med.) term are listed, with defibrillating being the participial adjective (ppl. a.) and defibrillator the noun. Carl Wiggers is a giant in cardiac electrophysiology, and the Lancet is one of the world’s leading medical journals.
electrotonus
The OED’s definition of electrotonus is different from mine.In IPMB, Russ and I write
The simplest membrane model is one that obeys Ohm’s law. This approximation is valid if the voltage changes are small enough so the membrane conductance does not change, or if something is done to inactivate the normal changes of membrane conductance with voltage. It is also useful for myelinated nerves between the nodes of Ranvier. This is called electrotonus or passive spread.IPMB says nothing about a constant current stimulus, and the OED says nothing about passive spread. I wonder if I’ve been using the word correctly? Wikipedia agrees with me.
The two vertical lines in the top left corner on the entry indicate an alien word (used in English, but from another language). I would have thought bremsstrahlung more deserving of this designation than electrotonus.
fluoroscope
Wilhelm Röntgen discovered x-rays in late 1895, so I’m surprised to see the term fluoroscope used only one year later. X-rays caught on fast. Nature is one of the best-known scientific journals.
leibniz
My PhD advisor John Wikswo and I are engaged in a quixotic attempt to introduce a new unit, the leibniz.If I were going to append a new definition, it would look something like this:
2. A unit corresponding to a mole of differential equations. 2006 HUANG et al. Rev. Physiol. Biochem. Pharmacol. CLVII. 98 Avogadro’s number of differential equations may be defined as one Leibnitz. 2006 WIKSWO et al. IEE P-Nanobiotechnol. CLIII. 84 It is conceivable that the ultimate models for systems biology might require a mole of differential equations (called a Leibnitz). 2015 HOBBIE and ROTH Intermediate Physics for Medicine and Biology 53 In computational biology, a mole of differential equations is sometimes called a leibniz.
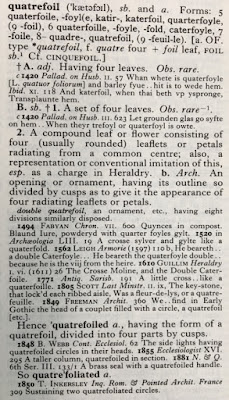
quatrefoil
Wikswo coined the term quatrefoil for four-fold symmetric reentry in cardiac tissue. Quatrefoil appears in the OED, but its definition is focused on foliage rather than heart arrhythmias. I guess Wikswo didn’t invent the word but he did propose a new meaning. I can’t complain that this sense of the word is missing from the OED, because quatrefoil reentry wasn’t discovered until after the second edition went to press. My proposed addition is:
3. A four-fold symmetric cardiac arrhythmia. 1999 LIN et al. J. Cardiovasc. Electrophysiol. X. 574 A novel quatrefoil-shaped reentry pattern consisting of two pairs of opposing rotors was created by delivering long stimuli during the vulnerable phase.
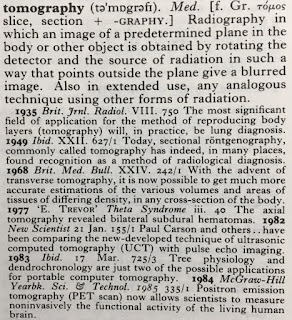
tomography
Godfrey Hounsfield built the first computed tomography machine in 1971. I didn’t realize that tomography had such a rich history before then. I don’t like the OED’s definition of tomography. I prefer something closer to IPMB’s: “reconstructing, for fixed z, a map of some function f(x,y) from a set of projections F(θ,x').”
Missing Words
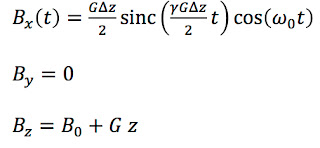
Some words from IPMB are not in the OED; for example chemostat, electroporation, and magnetosome. Kerma is absent, but it’s an acronym and they aren’t included. Brachytherapy is absent, even from the long entry for the prefix brachy-. Sphygmomanometer doesn’t have its own entry, although it’s listed among the surprisingly large number of words starting with the prefix sphygmo-. Magnetocardiogram is included under the prefix magneto-, but the more important magnetoencephalogram is not. I was hoping to find the definition of bidomain, but alas it’s not there. Here’s my version.bidomain (ˌbaɪdəʊ'meɪn). Phys. [f. BI- + -DOMAIN.] A mathematical description of the electrical behavior of syncytial tissue such as cardiac muscle. 1978 TUNG A Bi-domain Model for Describing Ischemic Myocardial D-C Potentials (Dissertation) 2 Bi-domain, volume-conductive structures differ from classical volume conductors (mono-domain structures) in that a distinction is made between current flow in the extracellular space and current flow in the intracellular space. 1983 GESELOWITZ and MILLER Ann. Biomed. Eng. XI. 200 The equations of the bidomain model are a three-dimensional version of the cable equations.
The OED took decades to complete, mostly during the Victorian era. The effort was led by James Murray, the hero of Winchester’s book. He supervised a small group of assistants, plus a motley crew of contributors whose job was to search English literature for examples of word use. Winchester’s stories about this collection of oddballs and misfits is engrossing; they volunteered countless hours with little recognition, some contributing tens of thousands of quotations, each submitted on a slip of paper during those years before computers. I can think of only one modern parallel: those unsung heroes who labor over Wikipedia.
 |
| The Professor and the Madman, by Simon Winchester. |
To close, I’ll quote the final paragraph of a speech that Prime Minister Stanley Baldwin gave in 1928 at a dinner celebrating the completion of the OED, which appears at the end of Winchester's Prologue to The Meaning of Everything.
It is in that grand spirit of devotion to our language as the great and noble instrument of our national life and literature that the editors and the staff of the Oxford Dictionary have laboured. They have laboured so well that, so far from lowering the standard with which the work began, they have sought to raise it as the work advanced. They have given us of their best. There can be no worldly recompense—expect that every man and woman in this country whose gratitude and respect is worth having, will rise up and call you blessed for this great work. The Oxford English Dictionary is the greatest enterprise of its kind in history.
 |
| Intermediate Physics for Medicine and Biology nestled among volumes of the Oxford English Dictionary. |