1.15 Diving
Air is easily compressible, so swimming at large depths can be dangerous as the volume of air in the lungs decreases. One can swim safely for depths of tens of meters (several atmospheres of pressure) using a self-contained underwater breathing apparatus (SCUBA). Compressed air tanks are used to supply air to the lungs, and the pressure of the air is adjusted to match the pressure of the surrounding water.
One physiological effect of breathing high-pressure air is that nitrogen dissolves into the blood, which can lead to a mental impairment known as nitrogen narcosis. Moreover, if the swimmer returns rapidly to the surface after a long deep dive, the lowered pressure allows the dissolved nitrogen to form bubbles in the blood that block blood flow and cause decompression sickness, often called “the bends” (Benedek and Villars 2000). To avoid the bends, swimmers must return to the surface slowly, or replace nitrogen by other gasses, such as helium, that are less soluble in blood.
 | |
| The Physics of Scuba Diving, by Marlow Anderson. |
Suppose [at a depth of 30 meters]… the diver fills his lungs with air [at 4 atm], and begins to ascend, while holding his breath. As the ambient pressure decreases, the air in the lungs expands. Since the diver is holding his breath, the air has nowhere to go, and so the flexible lung must expand in volume. If he were to hold his breath until reaching the surface, the lungs would have to expand to 4 times their original volume. Of course, this does not happen—instead, the lungs rupture, which can be an exceedingly dangerous injury. This leads to the number one principle drilled into divers when they train:
The Number One Rule of Scuba Diving
Any air cavity, not just the lungs, is at risk when diving. Another example is the ear. Anderson writesBreathe continuously, and never, never hold your breath.
When a scuba diver descends, pressure begins to build on the eardrum. In order to continue without pain or damage, this pressure must be counterbalanced by a corresponding pressure in the middle ear. However, ordinary respiration of pressurized air through the scuba regulator will not necessarily convey this needed pressure into the middle ear. Consequently, a typical diver must take action to push the pressurized air into these tiny spaces. Sometimes just a movement of the head and neck is enough to stretch the Eustachian tubes and bring this newly respirated (and pressurized) air into the middle ear. More often, however, the diver finds it necessary to perform a valsalva maneuver. This is an action many of us have taken to counteract the change of pressure experienced when flying in an airplane. Namely, you merely need to block the nostrils, and gently blow; the ears then “pop”. This is enough to move the air from the mouth and nostrils up the Eustachian tubes and into the middle ear. Scuba divers call this process equalization, for obvious reasons. You are taught in scuba training to equalize early, and often!Anderson then discusses another air pocket that I never thought of.
There is one more air space that must be equalized—the space between the [diving] mask and the eyes…It is for this reason that a diver’s mask includes the nostrils. The diver need only exhale through the nostrils into the mask in order to introduce the denser air with the appropriate pressure she has been breathing from the regulator. If the diver does not equalize this air space, the increasing ambient pressure at depth will push the mask even tighter against the face, eventually causing bruising… and this pressure can even burst the tiny capillaries in the eyes, making them bloodshot. But after only a little experience, divers equalize this air space almost without thinking about it.Gosh, scuba diving sounds complicated and even dangerous. I don’t think I’ll take up the sport.
The conduction and convection of heat also is important when diving. Russ and I discuss biological thermodynamics and heat transport in Chapters 3 and 4 of IPMB. In particular, we define the convection coefficient for heat loss in Homework Problem 51 of Chapter 3, when analyzing Newton’s law of cooling. The convection coefficient at the surface of our body is much larger in water than in air. Anderson notes
Convection can and does happen in the air too; this is especially true on a windy day, when the moving air continually replaces the air molecules that have been warmed by the body with cold ones: this is the origin of the concept of wind chill. However, the larger [thermal] conductivity of water makes this effect more powerful in water than in air. The practical consequence of this is that a diver in 80° [Fahrenheit] air can happily survive indefinitely. Our body continues to produce heat while turning food into energy. Some of this heat is lost to the surrounding air; indeed, we would quickly become overheated if we did not dissipate some of this energy. But in water of that same temperature more heat is lost than our body produces. The result is that the diver gets colder and colder. Indeed, a diver continually immersed even in warm tropical waters will eventually suffer from hypothermia. This is one of the major problems for divers lost at the surface.Yikes! Have you ever watched the end of the film Titanic?
Jack’s death scene in Titanic.
Another issue that arises under water is localizing the origin of sounds. Homework Problem 20 of Chapter 13 in IPMB says
Problem 20. People use many cues to estimate the direction a sound came from. One is the time delay between sound arriving at the left and right ears. Estimate the maximum time delay. Ignore any diffraction effects caused by the head.The solution’s simple: divide the distance between the ears by the speed of sound. Anderson explains
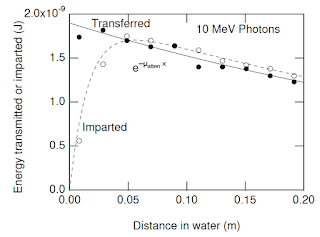
The four-fold increase in the speed of sound in water as compared to air means that our brain cannot as effectively detect the direction sounds come from! Hearing a boat motor overhead but being unable to determine the direction it is coming from is a common and frustrating experience for scuba divers.As you might expect, The Physics of Scuba Diving contains a long section about nitrogen absorption and the bends. Interestingly, the differential equation governing the absorption of nitrogen by the body is the same as described in Section 2.8 of IPMB: decay plus input at a constant rate. It is also the same equation governing Newton’s law of cooling
dP/dt = (Pa - P)/τ ,
where P is the partial pressure of nitrogen in the blood, Pa is the partial pressure of nitrogen being breathed (a function of depth), t is time, and τ is the time constant. Unfortunately, the process is complicated because the body contains several compartments, each with its own time constant.
It was the eminent British physiologist John Scott Haldane who first made use of the model for nitrogen on-gassing and off-gassing that we have described… His goal in understanding these rates was to help divers avoid the serious health effects of overly rapid decompressions… Haldane observed that various tissues in the body should be expected to have different rates of nitrogen absorption. A liquid (like blood) should be expected to very rapidly absorb nitrogen under pressure brought into contact with it. But a solid tissue like bone might be expected to absorb extra nitrogen at a much slower rate. Haldane consequently built a mathematical model to describe this. He assumed that body tissues could be put into five categories he called compartments, with different rates of absorption.Anderson then analyzes scuba dive tables using this model. He also gives some historical background about the bends, including an explanation about how the disease got its name.
The illness we call decompression sickness (or the bends) was first reported in the scientific literature in France in 1845, which a mining engineer named Charles-Jean Triger described the limb pain suffered by coal miners; he called their difficulties caisson disease… The mine had been filled with pressurized air to prevent ground water from entering the passages...My daughter Stephanie is taking scuba lessons, and plans on diving this summer at the Great Barrier Reef. Have fun, Stephanie, but be careful. Maybe she should read The Physics of Scuba Diving before she dives.
The construction (1869-1883) of the Brooklyn Bridge in New York was one of the engineering marvels of the nineteenth century. Massive caissons were constructed, including one as deep as 75 feet. Many workers suffered from caisson disease, including not only limb pain, but also paralysis and even death. The chief engineer for the project was stricken by the disease and remained paralyzed for the rest of his life [his wife took over the role of chief engineer, see David McCullough's wonderful book The Great Bridge]. It was during this period that the illness became popularly know as the bends, in reference to the exaggerated bending of the back workers attempted in a futile effort to avoid the pain. The name compared the posture of the bridge workers to the “Grecian Bend”, a posture adopted by fashionable women of the day.