Russ Hobbie and I describe magnetic resonance imaging in Chapter 18 of Intermediate Physics for Medicine and Biology. However, we don’t discuss the possibilities related to low-field MRI. The Science Happens! website says
Matthew Rosen and his colleagues at the Martinos Center for Biomedical Imaging in Boston want liberate the MRI. They’re hacking a new kind of scanner that’s fast, small, and cheap. Using clever algorithms, they can use a weak magnetic field to get good images of our brains and other organs. Someday, people may not have to go to hospital for an MRI. The scanners may show up in sports arenas, battlefields, and even the backs of ambulances.A longer, more technical video of Rosen describing his work is given below.
For more details, see Rosen’s open access article “Low-Cost High-Performance MRI” (Scientific Reports, 5:15177, 2015).
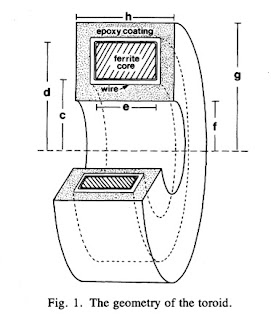
Magnetic Resonance Imaging (MRI) is unparalleled in its ability to visualize anatomical structure and function non-invasively with high spatial and temporal resolution. Yet to overcome the low sensitivity inherent in inductive detection of weakly polarized nuclear spins, the vast majority of clinical MRI scanners employ superconducting magnets producing very high magnetic fields. Commonly found at 1.5–3 tesla (T), these powerful magnets are massive and have very strict infrastructure demands that preclude operation in many environments. MRI scanners are costly to purchase, site, and maintain, with the purchase price approaching $1 M per tesla (T) of magnetic field. We present here a remarkably simple, non-cryogenic approach to high-performance human MRI at ultra-low magnetic field, whereby modern under-sampling strategies are combined with fully-refocused dynamic spin control using steady-state free precession techniques. At 6.5 mT (more than 450 times lower than clinical MRI scanners) we demonstrate (2.5 × 3.5 × 8.5) mm3 imaging resolution in the living human brain using a simple, open-geometry electromagnet, with 3D image acquisition over the entire brain in 6 minutes. We contend that these practical ultra-low magnetic field implementations of MRI (less than 10 mT) will complement traditional MRI, providing clinically relevant images and setting new standards for affordable (less than $50,000) and robust portable devices.$50,000 is expensive by Manu Prakash's standards, but for an MRI device $50k is darn cheap! Recalling my friend’s motto, I think that Rosen has picked Fast and Cheap, but he’s gotten Pretty Good too, which is not a bad trade-off (all of engineering is trade-offs). If you want Super Good, spend the million bucks.
Finally, Rosen isn’t the only one interested in reinventing magnetic resonance imaging. Michael Garwood at Russ’s own University of Minnesota is also working on smaller, lighter, cheaper MRI.
Let the race begin. Humanity will be the winner.
Enjoy!