|
My Die-Hard Cub Fan Club
membership card. |
Monday is
opening day!
When I was young I was an avid baseball fan. I still enjoy the game, but now I haven’t time to follow it closely. My childhood team was the
Chicago Cubs. I can still remember the lineup:
shortstop Don Kessinger led off,
second baseman Glenn Beckert hit next,
left fielder Billy Williams batted third, and
third baseman Ron Santo was
cleanup.
Ferguson Jenkins was the
pitching ace, colorful
Joe Pepitone—a former
Yankee—arrived by trade to play
first, Mr. Cub
Ernie Banks was in the twilight of his career, and hot-tempered
Leo Durochur was the
manager. The
Miracle Mets broke my heart in
1969, when the Cubs led their division into September only to collapse in the season's final weeks. The Cubs have not won the
World Series since
1908, but I still love ’em. Maybe this year?
I wasn’t a good
little league player;
I struck out a lot, and I was assigned to play
right field, where I could do the least damage with my glove. Yet, I had fun. One summer when I was in junior high, because of the timing of the age cutoffs and my birthday, I was nearly the oldest player in my age group. That was my best summer, when I approached mediocrity. I enjoyed the sport so much that I volunteered to manage the high school team. For those not familiar with baseball, being the manager in high school is very different than managing a professional team. In high school, the manager washes the uniforms, keeps track of the equipment, collects player statistics, and—my favorite job—draws the foul lines on the
field before each game.
 |
| Strat-O-Matic Baseball. |
When growing up in
Morrison, Illinois, my friend Ted Paul owned the game
Strat-O-Matic Baseball. It was played with
dice and player cards, allowing you to recreate baseball games from your armchair. Unfortunately, Strat-O-Matic Baseball was expensive. We were not poor, but the price was out of the range my parents spent on birthday or Christmas presents. Necessity is the mother of invention, so I reverse engineered the game, making my own cards and rules that mimicked Strat-O-Matic’s in some ways but in other ways were my own creation.
 |
Homemade Strat-O-Matic baseball cards
from the Oakland A’s, the dominant team
of that era (circa 1973). |
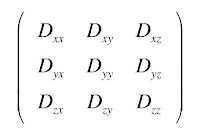
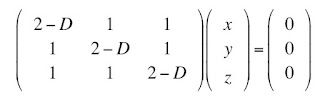
In order to make my version of Strat-O-Matic Baseball, I had to learn the basics of
probability. I didn’t need advanced concepts, and you can find all the necessary probability theory in Chapter 3 of
Intermediate Physics for Medicine and Biology. Two ideas are key. First, the probability that one or the other of two
mutually exclusive events happens is found by adding their individual probabilities. For instance, the probability of rolling either a one, two, or three on a single die is equal to the probability of rolling a one plus the probability of rolling a two plus the probability of rolling a three. Second, the probability that two
independent events both happen is found by multiplying their individual probabilities. For example, the probability of throwing a one on the first die and a three on the second is equal to the probability of throwing a one times the probability of throwing a three. This concept underlies the
joint probability distribution described in Appendix M of
IPMB. These two rules, plus some counting, is all the math required to recreate Strat-O-Matic baseball. I also needed a source of baseball statistics, supplied by
Street and Smith’s
Baseball Yearbook, published each year around
Valentine's Day and well within the family gift budget. In retrospect, making my own version of Strat-O-Matic Baseball was not difficult, but for a twelve-year-old kid I think I did a pretty good job.
Let me explain briefly how Strat-O-Matic Baseball works. The game was based on batters’ cards and pitchers’ cards. First you roll one die, and if you get a 1, 2, or 3 you use the batter’s card; a 4, 5, or 6 means you use the pitcher's card. Then you roll two dice which determine the outcome of the at-bat: out, walk, single, double, triple, or
home run. The trick is to match the player’s statistics to the probability of a particular throw of the dice. The pitchers’ cards were hardest to create, because Street and Smith didn’t tabulate batting averages given up by pitchers, so I had to invent an algorithm based on
wins,
earned run average, and
strikeouts. I remember spending many hours playing my homemade Strat-O-Matic baseball. In some ways it was pathetic: a child playing alone in his room with just his dice and cards. But in other ways it was romantic: thrilling late night ballgames with all the drama and excitement of sports, but performed just for me.
Even now, when I teach probability I focus on those key concepts I used when creating my version of Strat-O-Matic Baseball. Sometimes you learn more when you play than when you work.