|
| Introduction to Radiological Physics and Radiation Dosimetry, by Frank Herbert Attix. |
In his introduction, Attix discusses how small amounts of radiation can cause so much biological damage.
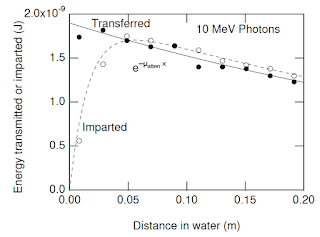
The reason why so much attention is paid to ionizing radiation, and that an extensive science dealing with these radiations and their interactions with matter has evolved, stems from the unique effects that such interactions have upon the irradiated material. Biological systems (e.g., humans) are particularly susceptible to damage by ionizing radiation, so that the expenditure of a relatively trivial amount of energy (~4 J/kg) throughout the body is likely to cause death, even though that amount of energy can only raise the gross temperature by about 0.001°C. Clearly the ability of ionizing radiations to impart their energy to individual atoms, molecules, and biological cells has a profound effect on the outcome. The resulting high local concentrations of absorbed energy can kill a cell...In Section 15.3 of IPMB, Russ and I analyze the photoelectric cross section, but don’t derive it from first principles. Attix writes
Theoretical derivation of the interaction cross section for the photoelectric effect is more difficult than for the Compton effect, because of the complications arising from the binding of the electron. There is no simple equation for the differential photoelectric cross section that corresponds to the K-N [Klein-Nishina] formula [relating the Compton cross section to the photon energy, hν]. However, satisfactory solutions have been reported by different authors for several photon energy regions…
The interaction cross section per atom for [the] photoelectric effect [τ], integrated over all angles of photoelectron emission, can be written as
τ = k Zn/(hν)m (cm2/atom)
where [Z is the atomic number,] k is a constant, n ~ 4 at hν = 0.1 MeV, gradually rising to about 4.6 at 3 MeV, and m ~ 3 at hν = 0.1 MeV, gradually decreasing to about 1 at 5 MeV.
In the energy region hν ~ 0.1 MeV and below, where the photoelectric effect becomes most important, it is convenient to remember that
τ ∝ Z4/(hν)3 (cm2/atom)...
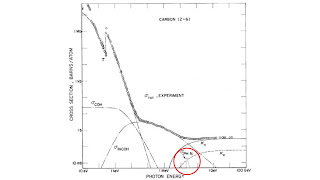 |
| Figure 15.2 of IPMB. The contribution of the photonuclear scattering cross section is circled in red. |
In a photonuclear interaction an energetic photon (exceeding a few MeV) enters and excites a nucleus, which then emits a proton or neutron. (γ, p) events contribute directly to the kerma, but the relative amount remains less than 5% of that due to pair production. Thus it has been commonly neglected in dosimetry considerations.
(γ, n) interactions have a greater practical importance because the neutrons thus produced may lead to problems in radiation protection…All of these consequences of (γ, n) interactions can be regarded as unwanted side effects of the use of higher-energy radiotherapy x-ray beams...Attix provides insight into the difference between how photons interact with tissue and how charged particles interact.
Charged particles lose their energy in a manner that is distinctly different from that of uncharged radiations (x- or γ-rays and neutrons). An individual photon or neutron incident upon a slab of matter may pass through it with no interaction at all, and consequently no loss of energy. Or it may interact and thus lose its energy in one or a few “catastrophic” events.Herb Attix was born in 1925 in Portland, Oregon, and served as a lieutenant in the navy during World War II. He was a professor at the University of Wisconsin, where he chaired the Department of Medical Physics before retiring in 1987. He has served on the board of directors for both the American Association of Physicists in Medicine and the Health Physics Society. In 1994 he received the William D. Coolidge Award, the highest award given by the AAPM.
By contrast, a charged particle, being surrounded by its Coulomb electric force field, interacts with one or more electrons or with the nucleus of practically every atom it passes. Most of these interactions individually transfer only minute fractions of the incident particle’s kinetic energy…A 1-MeV charged particle would typically undergo ~105 interactions before losing all of its kinetic energy.
The International Organization for Medical Physics marked its 50th anniversary by publishing short biographical sketches of 50 medical physicists who have made outstanding contributions to the advancement of medical physics over the last 50 years. You can read it here. Herb Attix was on the list. It reminds me of the NBA’s list of the top 50 players, but the IOMP honorees have contributed much more to mankind.